Asthma and Exercise-Induced Bronchospasm
This is an excerpt from Medical Conditions in the Physically Active 4th Edition With HKPropel Access by Katie Walsh Flanagan & Micki M. Cuppett.
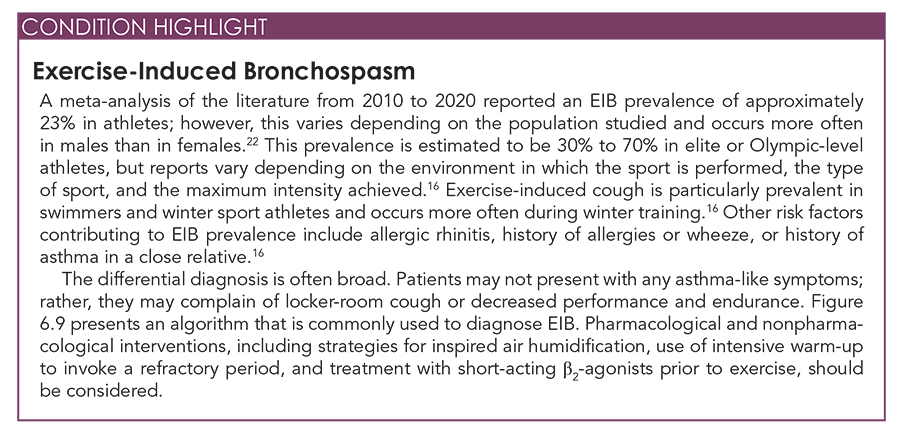
Airway disease is the most frequently encountered chronic respiratory condition in adolescents, affecting an estimated 8% of children and youths younger than age 18 yr in the United States. Several terms are often used to describe airway disease, especially if a definitive diagnosis has not yet been determined. Asthma, exercise-induced asthma (EIA), and exercise-induced bronchospasm (EIB) have been used interchangeably for many years; however, EIA is no longer a recommended term. EIB is defined as a transient narrowing of the lower airways after exercise in the presence or absence of clinically recognized asthma. Exercise triggers bronchoconstriction but does not induce the clinical syndrome of asthma.
Asthma occurs outside of exercise or strenuous activity and generally has two components that lead to obstruction: inflammation and spasm. Inflammation, characterized by mucosal edema and increased secretions, along with bronchospasm of smooth muscle, results in an increase in airway resistance and impeded airflow. Allergens, stress, anxiety, smoke and other environmental pollutants, cold ambient temperatures, and even exercise commonly trigger hyperreactivity of the airways. Asthma often begins in childhood and has various degrees of severity and progression. Some people require daily oral or inhaled medications, whereas others need only sporadic or intermittent treatment. Many patients do not have asthmatic symptoms except during strenuous exercise. Despite its various presentations, asthma can be life-threatening if not treated promptly and adequately.
Signs and Symptoms
Patients with airway disease (i.e., asthma and EIB) experience episodic, paroxysmal attacks of shortness of breath and wheezing as well as other symptoms, such as chest tightness and a dry cough. These episodes can be transient, lasting a few minutes to hours, or prolonged over several days. Severe attacks can be associated with substantial respiratory distress and tachypnea. Wheezing may be audible to the unaided ear in some cases. Mild cases may present as only a chronic cough (cough variant asthma). In the general population, particularly among individuals with asthma, cough is a common symptom. In athletes, exercise-induced cough is a particularly frequent symptom that presents after activity and is often termed locker-room cough.
In patients suspected of having EIB, another important differential diagnosis is exercise-induced laryngeal obstruction (EILO), in which wheezing and dyspnea are caused by transient obstruction of the upper airways during exercise. EIB should be suspected in any patient who complains of shortness of breath, dyspnea, cough, chest congestion, or tightness with exertion. Symptoms of EIB usually occur 10 to 15 min after onset of strenuous exercise and are defined by a decrease of 15% or more in forced expiratory volume within the first second (FEV1) during exercise spirometry. EIB is more common in winter sport athletes who compete in cold ambient temperatures.
Asthma and EIB should be differentiated from other upper and lower respiratory diseases, such as acute sinusitis, otitis media (middle ear infection), bronchitis, or even pneumonia, particularly in the context of other constitutional symptoms, such as fever, chills, or night sweats. More serious cardiac causes, such as arrhythmia and pericarditis, may also need to be excluded, including EILO, croup, infiltrative lung disease, and even foreign body aspiration. If fatigue is the only presenting symptom, deconditioning may also be a cause. In addition, environmental allergies can account for many of the nonspecific symptoms that mimic EIB. The examiner must always consider cardiac failure, chronic obstructive pulmonary disease (COPD), or airway tumors as differential diagnoses in older patients, especially smokers. Determining whether the condition is asthma (occurs at rest) or EIB (only occurs with exercise) is helpful. The Global Initiative for Asthma (GINA) guidelines outline several symptoms that increase or decrease the probability of a patient having asthma. For example, symptoms that worsen at night or in the early morning, that vary over time and in intensity, and that are triggered by exercise, irritants, and allergens increase the probability of asthma.
Both respiratory rate and heart rate may be elevated on examination, depending on the severity of the condition. In particular, the use of accessory muscles of respiration may be seen during respiratory distress. The sternocleidomastoid, trapezius, and levator muscles contract during respiratory distress, giving patients the appearance of lifting their shoulders as they breathe. On auscultation, wheezes are usually present, particularly during expiration. The expiratory phase is also prolonged as airway resistance is increased. Breath sounds can be diminished.
Referral and Diagnostic Tests
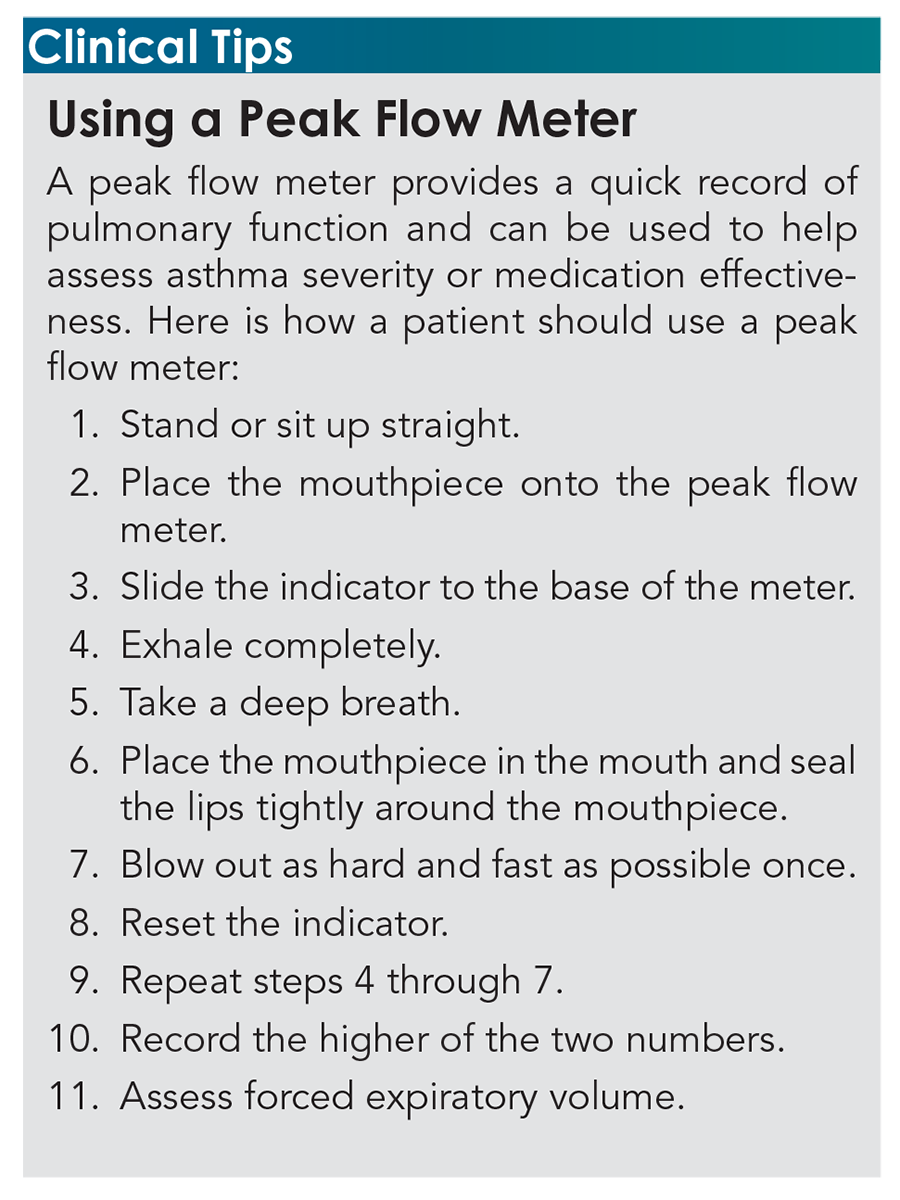
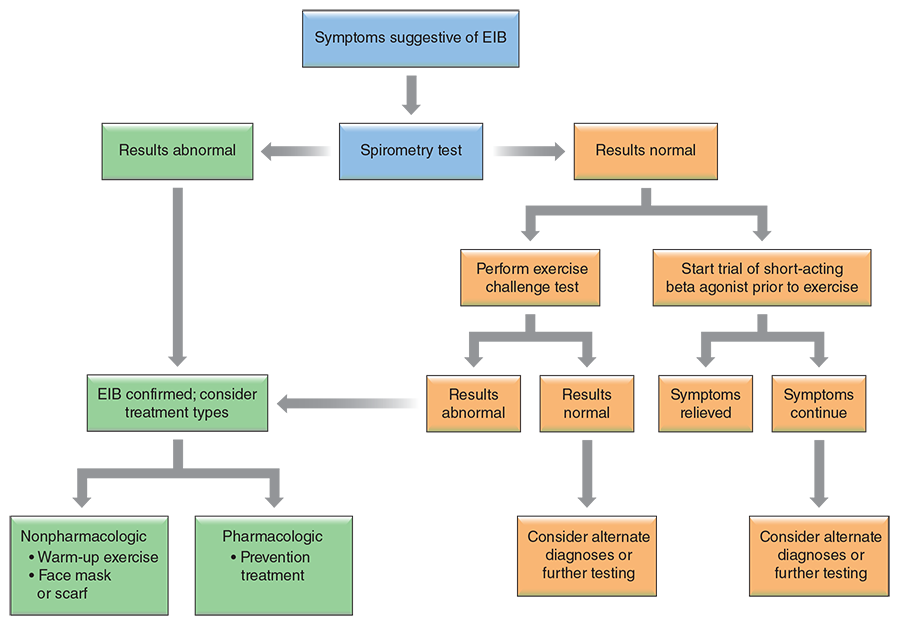
Resting spirometry measurements are generally poor predictors of variable airflow obstruction in athletes, because their lung function at rest is typically greater than that of the general population. If both the patient history and examination suggest asthma, response to empirical treatment with a β-agonist such as albuterol is often diagnostic. A decrease in predicted FEV1 measured by spirometry, particularly in response to cholinergics such as methacholine (i.e., the methacholine challenge test), is considered the gold standard for diagnosis. The physical examination is usually normal in an athlete with EIB. Some athletes may experience symptoms that develop several hours after exercise. This late-phase response is attributable to the activity of inflammatory mediators. Use of repeated spirometry after exercise can be helpful in the diagnosis of EIB. Most commonly, an exercise challenge or bronchial provocation test is used to determine the diagnosis of EIB.Because of the lack of simple, standardized diagnostic methods, underdiagnosis and misdiagnosis of EIB are common. Symptom-based questionnaires have been used to assist with diagnosis of EIB but have not been validated to date. Figure 6.9 presents a decision tree commonly used for the diagnosis of EIB. Alternatively, many physicians choose to just evaluate the patient’s response to an empirical trial of a β-agonist before exercise.
Inhaled β-agonists, both long and short acting, are mainstays in the treatment of asthma. Other medications used to treat asthma include oral and inhaled steroids, mast cell stabilizers such as cromolyn, leukotriene modifiers, and theophylline. Treatment recommendations generally follow a stepwise approach in the use of both rescue and maintenance medications as disease severity dictates. A large body of evidence supports use of the long-acting antimuscarinic tiotropium bromide (e.g., Spiriva) for asthma, and this medication is now recommended in current international GINA guidelines for chronic treatment of patients older than age 12 yr with the most severe and frequently exacerbated forms of the disease. Refer to chapter 4 for a complete description of asthma medications and indications. In addition to pharmacotherapy, attention must be given to the avoidance of known triggers and the treatment of concomitant allergies. Although strenuous exercise can provoke airway disease, several studies have shown that regular exercise and improvement in physical fitness (specifically pulmonary function) may reduce symptoms and airway irritability.
In general, patients and athletes with mild asthma may participate in most sports. However, because cold ambient temperatures exacerbate asthma symptoms, many prefer sports that involve competition in warm, temperate climates, such as track and field. Individuals with moderate to severe asthma are unlikely to be involved in vigorous athletic activities because the disease often limits performance. Patients with acute exacerbations of asthma should refrain from activity until the acute attack resolves and they no longer need rescue medications (e.g., albuterol) regularly.
Treatment for EIB is similar to that for asthma, with the patient using a metered-dose inhaler to administer a β2-agonist (e.g., albuterol) 15 to 30 min before exercise onset. A patient who has asthma symptoms outside the exercise setting or uses a β2-agonist more than three times per week should be treated with a regular inhaled corticosteroid. For proper use of a metered-dose inhaler, see chapter 4.
Studies show promise with the use of long-acting β2-agonists (e.g., salmeterol) and leukotriene inhibitors (e.g., montelukast; Singulair). Other nonpharmacological strategies include pre–warm-up bursts of physical activity at 80% to 90% of the individual’s maximal workload to induce a refractory period that lasts up to 3 h after the initial EIB attack. Dietary interventions and strategies to humidify inspired air may also be beneficial.
For a patient experiencing a severe asthma attack or ineffective inhaler treatment, a nebulizer (or atomizer) may be used. The nebulizer machine vaporizes liquid medication into a fine mist that is inhaled into the lungs via a mouthpiece or mask. Although studies have shown that both inhalers and nebulizers tend to be equally effective in delivering medication, nebulizers are preferred in more serious rescue situations when the patient is experiencing a severe asthma attack. Nebulizers can administer a higher dose of medication, but inhalers are easier to use, preferred for their portability and low cost, and considered suitable for everyday use. Medications typically administered with a nebulizer include albuterol and ipratropium (Atrovent).
Patients with controlled EIB need not be excluded or discouraged from participating in sports. Effective strategies, both pharmacological and nonpharmacological, exist that can allow an athlete to compete, even at an elite level.
SHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW


